Seamless Integration with Electronic Health Records (EHR) Systems
Core Insights
Seamless integration with Electronic Health Records (EHR) systems allows healthcare applications to securely exchange patient data, improve clinical workflows, and enhance care delivery. By utilizing interoperability standards like FHIR and HL7, and connecting through standardized APIs, healthcare apps can provide real-time access to medical records while ensuring compliance with privacy regulations such as HIPAA. This guide explores the essential components, from secure data access to user authentication, for building reliable, scalable EHR integrations that meet the evolving demands of modern healthcare.
Why EHR Integration Matters for Healthcare Apps
Electronic Health Records (EHRs) are the digital foundation of modern clinical practice. Healthcare apps that lack integration with EHR systems often result in fragmented workflows, manual data entry, and missed opportunities to improve patient care.
When your app integrates directly with EHR platforms like Epic, Oracle Health, or Veradigm, it gains real-time access to critical data such as:
- Patient demographics and history
- Medication and allergy lists
- Lab results and imaging reports
- Appointment schedules and provider notes
This integration not only enhances clinical decision-making but also streamlines administrative tasks like scheduling, billing, and patient communication.
Key Benefits of EHR Integration:
- Faster access to complete patient information
- Streamlined care coordination across departments
- Reduced administrative burden for clinical staff
- Improved outcomes through timely, data-informed decisions
As healthcare becomes more digital and data-driven, seamless EHR integration is essential for delivering efficient, patient-centered care.
What Is EHR Integration? (And How It Works)
EHR integration refers to the process of connecting healthcare applications to Electronic Health Record (EHR) systems in order to securely exchange patient data. Through this connection, apps can read from and write to EHRs, enabling real-time access to clinical information, improving workflows, and enhancing care coordination.
Simply put, it’s about embedding apps directly into clinical ecosystems where they can inform decision-making and automate tasks.
Here’s how EHR integration works:
- APIs (Application Programming Interfaces): Most major EHR platforms expose APIs (such as FHIR) that allow third-party apps to interact with patient data securely.
- Standards-Based Data Exchange: Interoperability standards like HL7 v2 and FHIR ensure consistent data formatting across systems.
- Secure Access Controls: Authentication protocols like OAuth 2.0 and SAML are used to verify users and manage data access permissions.
- Bidirectional Syncing: Healthcare apps can retrieve patient history, lab results, and appointments, as well as push back updates such as completed forms or provider notes.
By building on these foundations, EHR-integrated apps become trusted extensions of the clinical system, supporting care without disrupting workflow.
Standards-Based Data Exchange (FHIR, HL7)
To ensure compatibility and efficiency across systems, most healthcare apps rely on interoperability standards like FHIR (Fast Healthcare Interoperability Resources) and HL7 v2.
Why Use HL7 or FHIR?
- Widely adopted by major EHR platforms
- Support secure, structured data exchange
- Reduce custom integration efforts
- Enable app scalability across different vendors
FHIR supports modern API formats (JSON/XML) and is especially useful for mobile and web apps. HL7, while older, is still the foundation of messaging in labs and hospitals.
Leveraging EHR APIs for Real-Time Syncing
APIs are the engines of integration. They allow apps to access and interact with EHR data in real time. Most EHR vendors, including Epic, Cerner, and athenahealth, offer FHIR-based APIs.
Common API Actions:
- GET /Patient/{id}: Retrieve patient demographics
- POST /Observation: Submit new lab results or vitals
- PATCH /Appointment: Update scheduling information
This real-time exchange allows apps to:
- Display current medications before a virtual consult
- Push completed pre-visit forms into the EHR
- Notify providers about patient-reported symptoms
Pro Tip: Check if your vendor supports Bulk FHIR Export for population health applications.
Improve Workflow with Single Sign-On (SSO)
Single Sign-On (SSO) enables healthcare providers to use one set of credentials to access both the EHR and integrated applications. It greatly enhances clinician workflow by reducing the need for multiple logins.
Benefits of SSO Integration:
- Unified login across systems
- Reduced login time and errors
- Faster user adoption and onboarding
According to NIST guidelines, SSO also supports secure identity management across platforms.
Consent and Role-Based Access Control (RBAC)
To ensure patient data is accessed securely and legally, healthcare apps must implement:
- Explicit patient consent: Logged and documented
- Role-Based Access Control (RBAC): Access limited by user role
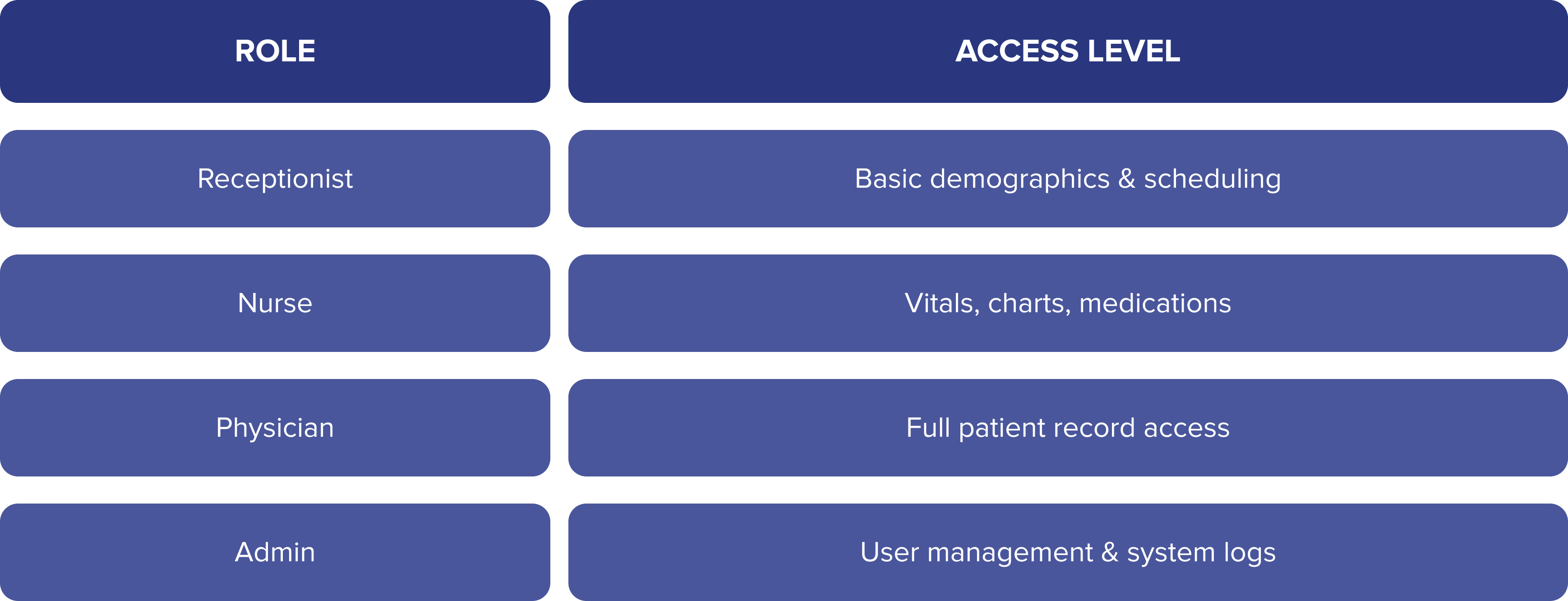
Complying with the HIPAA Security Rule requires audit trails, encryption, and controlled data access.
Data Mapping and Normalization
EHRs may use different data formats, naming conventions, and coding standards. Mapping and normalization ensure that information flows correctly between systems.
Common Mapping Challenges:
- ICD-10 vs SNOMED coding systems
- Units of measurement inconsistencies (e.g., mg/dL vs mmol/L)
- Varying date/time formats
Pro Tip: Use standardized terminologies like LOINC for labs and RxNorm for medications.
Error Handling and Integration Logging
No integration is perfect, which is why robust error handling and logging are essential.
What to Log:
- Timestamps of sync attempts
- API call responses (success/failure)
- Error codes and diagnostics
- Data successfully transferred or rejected
These logs not only aid in troubleshooting but also support compliance audits and usage analytics.
Collaborate with EHR Vendors During Development
EHR vendors typically have their own rules, sandbox environments, and documentation. Engaging early with them ensures smooth integration.
Integration Checklist:
✅ Request sandbox/test environment access
✅ Review API rate limits and security policies
✅ Confirm authentication method (OAuth 2.0, SAML, etc.)
✅ Clarify consent flow requirements
Pro Tip: Explore resources like Epic App Orchard or Cerner Ignite for platform-specific guidance.
Final Thoughts: Future-Proofing EHR Integrations
EHR integration nowadays is an absolute strategic necessity. |
As healthcare becomes more data-driven, apps that use standards like FHIR and build on secure APIs will be best positioned for:
- Scalable growth
- Enhanced patient outcomes
- Cross-platform interoperability
By prioritizing seamless, standards-based integration, your healthcare app becomes a trusted part of the care continuum. For further guidance, consult the 21st Century Cures Act and the ONC Interoperability Roadmap.