Real-Time Communication in Healthcare: How Providers and Patients Stay Connected
Core Insights
Real-time communication in healthcare means enabling instant, secure interactions between patients and providers through messaging, video, voice calls, and file sharing. These tools improve patient outcomes, reduce delays in care, and increase patient engagement by making medical support accessible anytime. By combining secure messaging, telemedicine video consultations, VoIP calling, and HIPAA-compliant file sharing with real-time alerts and availability indicators, healthcare apps can deliver seamless and efficient communication. In this article, we’ll explore how healthcare organizations can build and optimize real-time communication systems that meet privacy standards while improving care delivery.
New Standard in Healthcare: Real-Time Communication
Imagine a patient experiencing sudden chest discomfort late at night. Instead of waiting until morning or rushing to the ER, they open a healthcare app, send a secure message, and within minutes, a provider responds through a quick video consultation. The doctor reviews the patient’s recent test results, gives immediate guidance, and determines whether an in-person visit is necessary. What could have been a night of fear becomes a moment of reassurance, all thanks to real-time communication.
Stories like this highlight why real-time patient-provider communication has become the backbone of modern healthcare.
Timely exchanges between patients and clinicians:
- Prevent delays in diagnosis and treatment
- Reduce medical errors caused by miscommunication
- Keep patients engaged and satisfied with their care
- Support smoother coordination across healthcare teams
As telehealth adoption accelerates, the ability to connect instantly is no longer a luxury.
Secure Messaging: The Foundation of Trust
At the heart of digital communication is secure messaging. For many patients, being able to send a quick question to their doctor or receive follow-up instructions in writing is incredibly reassuring. But because these exchanges involve sensitive health information, the messaging system must be built with robust protections.
End-to-end encryption ensures that only the patient and provider can access the content. HIPAA compliance safeguards the platform against unauthorized use and establishes trust. Secure storage prevents accidental data exposure, while access controls allow providers to manage conversations across multiple patients safely.
Secure messaging also supports continuity of care. A patient recovering from surgery can ask about side effects, a parent can clarify dosage instructions for a child, or a nurse can provide routine updates – all without the delays of scheduling an appointment. By making communication simple yet compliant, secure messaging lays the groundwork for stronger provider-patient relationships.
Video Conferencing for Telemedicine
While messaging is useful for quick exchanges, sometimes a face-to-face interaction is essential. Video conferencing allows providers to visually assess symptoms, build rapport, and conduct remote consultations that feel personal and comprehensive.
Telemedicine video conferencing platforms typically rely on technologies like WebRTC or dedicated APIs to ensure stable, high-quality video calls. These tools make it possible for doctors to “see” patients even when they are miles apart. For patients in rural areas or those with mobility challenges, this kind of accessibility is transformative.
The benefits are broad:
- Convenience – patients avoid travel, saving time and money
- Expanded access – specialists can consult across regions and time zones
- Reduced no-shows – digital visits lower barriers to attendance
- Continuity – chronic disease management becomes easier with frequent virtual check-ins
In short, video conferencing brings the doctor’s office to wherever the patient is.
Voice Calling for Seamless Accessibility
Not every patient has the bandwidth or technology for video consultations, and not every scenario requires it. Voice calling offers a practical alternative that is often more inclusive.
For elderly patients who may find video technology intimidating, a simple call is more accessible. In regions with unreliable internet connections, VoIP-based voice services ensure communication remains possible. Providers can deliver quick advice or reassurance without the need for complex tools.
In healthcare, accessibility matters as much as innovation. Offering multiple communication modes ensures no patient is left behind.
File and Image Sharing for Better Care
Healthcare communication is not limited to words. Patients often need to share documents or images (e.g., a blood test report, an X-ray scan, or a photo of a skin condition). Secure file and image sharing makes this possible in real time.
For providers, the ability to quickly review lab results or images can speed up diagnoses. For patients, it reduces the stress of waiting. Imagine being able to upload a scan directly through the app and receive feedback within hours, rather than days.
To be effective, file sharing must support common medical formats like PDFs, JPEGs, and even DICOM images. Encryption and access control ensure files remain confidential, while compatibility across devices keeps the process smooth for both sides.
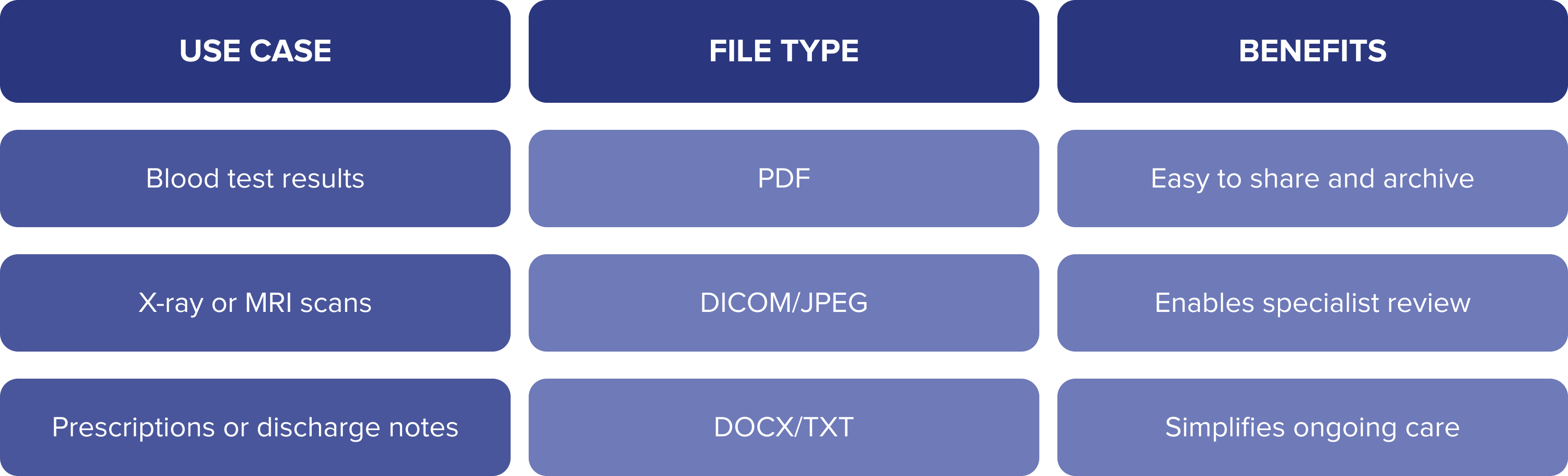
By making secure file sharing a core feature, healthcare apps empower patients and providers to exchange critical information without delays.
Push Notifications & Real-Time Alerts
Timely communication doesn’t always require a direct exchange. Push notifications are a simple yet powerful way to keep patients engaged and informed.
Appointment reminders reduce no-shows and keep clinics running smoothly. Medication alerts support adherence, which is especially valuable for patients managing chronic conditions. Real-time health updates, such as lab results becoming available, reassure patients that their care is progressing.
Studies show that patients who receive reminders are far more likely to stay on track with their treatment. In this sense, push notifications aren’t just administrative tools; they directly contribute to better health outcomes.
Presence & Availability Indicators
Have you ever sent a message and wondered when you’ll get a reply? For patients, that uncertainty can be stressful. Presence and availability indicators solve this problem by showing whether a provider is online, offline, or available for immediate consultation.
This transparency helps set realistic expectations. Patients know when to anticipate a response, while providers can manage their workloads without feeling pressured to reply instantly at all hours. For urgent cases, availability indicators provide reassurance that help is only a message away.
Multimodal Communication: Flexibility for Every Patient
Every patient is different. Some are comfortable with written messaging, others prefer talking over the phone, and complex cases may require video consultations. A multimodal platform brings all these options together in a single, seamless experience.
The ability to switch between communication modes ensures flexibility. A patient might start with a secure message, escalate to a voice call for clarification, and then move to a video consultation if visual assessment is needed. By offering multiple pathways, healthcare providers make sure patients feel supported in the way that suits them best.
Compliance & Security: Meeting HIPAA Standards
Behind every communication feature lies the critical responsibility of compliance. The Health Insurance Portability and Accountability Act (HIPAA) sets strict standards for protecting patient health information, and any real-time communication system must meet them.
Key safeguards include:
- Encryption of data at rest and in transit
- Role-based access controls to limit exposure
- Audit trails to monitor activity and ensure accountability
- Consent mechanisms so patients know how their data is used
By embedding these safeguards into the communication infrastructure, healthcare organizations can maintain trust and ensure their digital tools are both innovative and responsible.
Building the Future of Patient-Provider Communication
Real-time communication is redefining how patients and providers connect. From secure messaging and video calls to file sharing, push notifications, and multimodal platforms, these tools are creating healthcare experiences that are faster, safer, and more patient-centered.
As digital care continues to grow, organizations that invest in reliable, HIPAA-compliant communication tools will not only improve clinical outcomes but also strengthen the relationships at the heart of medicine. In the future, patients are simply going to demand them.